Ministry of Health and Family Welfare
Saving Mothers, Strengthening Futures
India’s Success in Reducing Maternal Mortality
Posted On:
21 MAR 2025 6:41PM by PIB Delhi
Introduction
Maternal mortality remains a critical public health issue in India. It serves as a key indicator of healthcare quality and accessibility, reflecting the effectiveness of maternal health services. Maternal death is the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes. Addressing maternal mortality is essential for ensuring the well-being of women and newborns and achieving global health goals.

One of the key indicators of maternal mortality is the Maternal Mortality Ratio (MMR) which is defined as the number of maternal deaths during a given time period per 100,000 live births during the same time period. India has made commendable progress in reducing maternal mortality, with the MMR declining from 130 per 100,000 live births in 2014-16 to 97 per 100,000 live births in 2018-20. This decline can be attributed to various government initiatives, improved healthcare access, and better medical interventions.
Trends in Maternal Mortality in India
On May 15, 2015, World Health Organisation (WHO) certified India for eliminating maternal and neonatal tetanus. Maternal mortality trends in India also show a steady decline over the years.

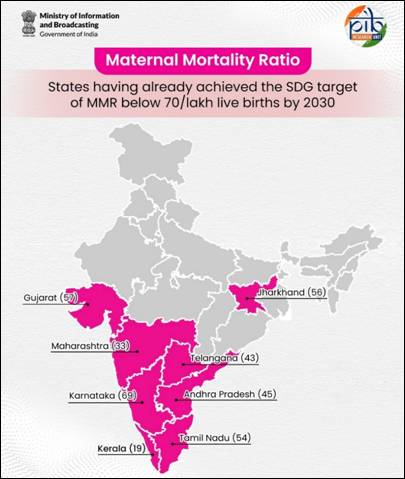
While some states have successfully reduced their MMR to levels below the SDG target of 70 per 100,000 live births, others still struggle with high maternal deaths. Eight states—Kerala, Maharashtra, Telangana, Andhra Pradesh, Tamil Nadu, Jharkhand, Gujarat, and Karnataka—have already achieved this SDG target.
According to the latest National Family Health Survey-5 (2019-21) report:
• The proportion of pregnant women who had an Antenatal Care (ANC) visit in the first trimester increased from 59% in NFHS-4 (2015-16) to 70% in NFHS-5 (2019-21).
• At the national level, there is an increase from 51% (2015-16) to 59% (2019-21) of women receiving the recommended four or more ANC visits from health providers.
• Institutional births have increased significantly from 79% (2015-16) to 89% (2019-21) at the national level. Institutional delivery is 100% in Kerala, Goa, Lakshadweep, Puducherry and Tamil Nadu and more than 90% in eighteen other States/UTs.
• Even in rural areas, approximately 87% of births are delivered in institutions, while 94% are delivered in urban areas.
|
Age Distribution of Maternal and Non-Maternal deaths, India, 2018-20
|
|
Age Group
|
Maternal Deaths
|
Non-maternal Deaths
|
|
15-19
|
6%
|
9%
|
|
20-24
|
32%
|
11%
|
|
25-29
|
30%
|
12%
|
|
30-34
|
20%
|
13%
|
|
35-39
|
8%
|
14%
|
|
40-44
|
3%
|
18%
|
|
45-49
|
2%
|
22%
|
Government Initiatives to Reduce MMR
India has committed to the UN target for Sustainable Development Goal (SDG) for MMR at 70 per 1,00,000 live births by 2030 and NHP (National Health Policy) 2017 target for MMR less than 100 per 1,00,000 live births by 2020. India has accomplished the National Health Policy (NHP) target for MMR.
The Ministry of Health and Family Welfare (MoHFW) supports all States/UTs in implementation of Reproductive, Maternal, New-born, Child, Adolescent health and Nutrition (RMNCAH+N) strategy under National Health Mission (NHM) based on the Annual Programme Implementation Plan (PIP) submitted by States/ UTs to reduce MMR & Neonatal Mortality Rate. To address maternal mortality, the Indian government has implemented various policies and schemes aimed at improving maternal healthcare. These programs focus on increasing institutional deliveries, enhancing healthcare infrastructure, and ensuring timely interventions for high-risk pregnancies.
National Health Mission (NHM) and Maternal Health
The National Health Mission (NHM) plays a crucial role in India’s efforts to reduce maternal mortality. It includes the Reproductive, Maternal, Newborn, Child, Adolescent Health, and Nutrition (RMNCAH+N) strategy, which encompasses multiple programs to improve maternal health outcomes. Key programs under NHM include:
- Janani Suraksha Yojana (JSY): Launched in 2005 with the objective of reducing maternal and neonatal mortality, JSY promotes institutional delivery among pregnant women especially with weak socio-economic status i.e. women from Scheduled Castes, Scheduled Tribes and BPL households.
- Pradhan Mantri Matru Vandana Yojana (PMMVY), is a maternity benefit program run by the Ministry of Women and Child Development, Government of India. The maternity benefit, of Rs. 5000/-, is available to a woman for the first living child of family subject to fulfilment of conditionalities. All Pregnant Women who have their pregnancy for the first child in family on or after 01.01.2017 are eligible for getting benefit under the programme. Further, as per the new guideline for 'Mission Shakti’, applicable with effect from 01.04.2022, the scheme (PMMVY 2.0) seeks to promote positive behavioural change towards girl child by providing additional cash incentive for the second child, if that is a girl child.
- Janani Shishu Suraksha Karyakaram (JSSK): Launched in 2011, JSSK aims at eliminating out-of-pocket expenses for pregnant women and sick infants by entitling them to free delivery, including caesarean section, free transport, diagnostics, medicines, other consumables, diet and blood in public health institutions.
- Surakshit Matritva Aashwasan (SUMAN): Launched in 2019, SUMAN aims to provide assured, dignified, respectful and quality healthcare at no cost and zero tolerance for denial of services for every woman and new-born visiting the public health facility to end all preventable maternal and new-born deaths.
- Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA): Launched in 2016, PMSMA provides pregnant women a fixed day, free of cost assured and quality Antenatal Care on the 9th day of every month. Further, Extended PMSMA (e-PMSMA) strategy is implemented to ensure quality ANC to pregnant women, especially to high-risk pregnancy (HRP) women and individual HRP tracking till a safe delivery is achieved by means of financial incentivization for the identified high risk pregnant women and accompanying ASHA for extra 3 visits over and above the PMSMA visit. As on March 21, 2025, more than 5.9 crore pregnant women have been examined under this scheme.
- LaQshya: Launched in 2017, LaQshya aims to improve the quality of care in labour room and maternity operation theatres to ensure that pregnant women receive respectful and quality care during delivery and immediate post-partum.
- Capacity building is taken-up for MBBS doctors in Anesthesia (LSAS) and Obstetric Care including C-section (EmOC) skills to overcome the shortage of specialists in these disciplines, particularly in rural areas.
- Maternal Death Surveillance Review (MDSR) is implemented both at facilities and at the community level. The purpose is to take corrective action at appropriate levels and improve the quality of obstetric care.
- Monthly Village Health, Sanitation and Nutrition Day (VHSND) is an outreach activity for provision of maternal and child care including nutrition.
- Regular IEC/BCC is conducted for early registration of ANC, regular ANC, institutional delivery, nutrition, and care during pregnancy etc.
- MCP Card and Safe Motherhood Booklet are distributed to the pregnant women for educating them on diet, rest, danger signs of pregnancy, benefit schemes and institutional deliveries.
- Reproductive and child health (RCH) portal is a name-based web-enabled tracking of pregnant women and new-born to ensure provision of regular and complete services to them including antenatal care, institutional delivery and post-natal care.
- Anaemia Mukt Bharat (AMB) strategy as a part of POSHAN Abhiyan aims to strengthen the existing mechanisms and foster newer strategies to tackle anaemia which include testing & treatment of anaemia in school going adolescents & pregnant women, addressing non-nutritional causes of anaemia and a comprehensive communication strategy.
Infrastructure Strengthening
Strengthening healthcare infrastructure is a key strategy in reducing maternal mortality. Investments in medical facilities and personnel training enhance the quality of maternal healthcare services. Several measures have been taken to improve healthcare infrastructure:
- Comprehensive Abortion Care (CAC) services are strengthened through trainings of health care providers, supply of drugs, equipment, Information Education and Communication (IEC) etc.
- Delivery Points- ‘Delivery Points’ have been strengthened in terms of infrastructure, equipment, and trained manpower for provision of comprehensive RMNCAH+N services
- Functionalization of First Referral Units (FRUs) by ensuring manpower, blood storage units, referral linkages etc.
- Setting up of Maternal and Child Health (MCH) Wings at high caseload facilities to improve the quality of care provided to mothers and children.
- Operationalization of Obstetric ICU/HDU at high case load tertiary care facilities across country to handle complicated pregnancies.
Success Stories and Innovations in Maternal Healthcare
India has witnessed a remarkable success in reducing maternal mortality through innovative healthcare strategies and targeted interventions. These success stories serve as a model for further progress and inspiration for other regions.
Several states have pioneered unique initiatives that have significantly contributed to reducing maternal mortality, including:
- Madhya Pradesh’s 'Dastak Abhiyan': A community-driven campaign that focuses on early detection of maternal health risks and ensures timely medical intervention.
- Tamil Nadu’s Emergency Obstetric Care Model: A robust referral system that ensures pregnant women receive timely emergency care, reducing maternal complications.
By building on these success stories and adopting innovative approaches, India is on the right path to achieving further reductions in maternal mortality and ensuring safer pregnancies for all women. To further reduce maternal mortality, India must continue strengthening healthcare systems, enhancing policies, and expanding access to quality maternal health services.
Conclusion
India has made significant progress in reducing maternal mortality, successfully achieving the National Health Policy (NHP) target of an MMR below 100 by 2020. However, continued efforts are required to reach the SDG target of MMR below 70 by 2030. Strengthening healthcare infrastructure, expanding maternal health programs, and addressing socioeconomic barriers will be critical in further reducing maternal mortality in the country.
References
https://pmsma.mohfw.gov.in/
https://mohfw.gov.in/?q=hi/node/8491
https://tncea.dmrhs.tn.gov.in/program/CEmOC.pdf
https://censusindia.gov.in/nada/index.php/catalog/44379
https://pib.gov.in/PressReleasePage.aspx?PRID=1575157
https://sansad.in/getFile/annex/259/AU2341.pdf?source=pqars
https://mohfw.gov.in/sites/default/files/Final.pdf
https://prc.mohfw.gov.in/fileDownload?fileName=.pdf
See in PDF
***
Santosh Kumar | Sarla Meena | Rishita Aggarwal
(Release ID: 2113800)
Visitor Counter : 20553