PIB Headquarters
Leprosy in India: The Road to a Disease-Free Future
प्रविष्टि तिथि:
05 OCT 2025 11:12AM by PIB Delhi
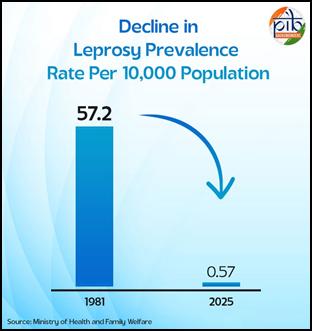
- India’s leprosy prevalence rate has fallen from 57.2 per 10,000 population in 1981 to just 0.57 in 2025.
- Among the new cases detected, percentage of child cases has dropped from 9.04% in 2014-15 to 4.68% in 2024-25.
- As of March 2025, 31 states and 638 districts have achieved a prevalence rate of less than 1 per 10,000 population, sustaining India’s elimination status nationally.
|
Leprosy, or Hansen’s disease, is a chronic infectious disease caused by bacteria Mycobacterium leprae. Infection can lead to involvement of the nerves, respiratory tract, skin, and eyes. Symptoms include discoloured skin patches, lack of ability to feel touch, pressure, pain, heat and cold, muscle weakness, non-healing ulcers, deformities particularly in hands, feet and face and inability to close eyes and poor vision. Leprosy is transmitted through droplets from the nose and mouth during close and frequent contact with untreated cases. The disease is feared because it can lead to deformity; this is also the cause of the social stigma traditionally attached to the disease. Leprosy can be multibacillary or paucibacillary. While multibacillary leprosy shows a high density of bacilli on slit-skin smear examination, paucibacillary leprosy cases show only a few or no bacilli on slit-skin smear examination. The introduction of Multidrug Therapy (MDT) in 1983 in India revolutionized treatment of leprosy. MDT treatment has been provided free of cost to patients through WHO. Early diagnosis and treatment with MDT can prevent disabilities and deformities. Since the introduction of MDT, the incidence and prevalence of the disease has remarkably decreased. (World Health Organization [WHO], 2024).
The Situation in India Since Independence
Decennial population census of 1951 reported 13,74,000 and a prevalence rate of 38.1 per 10,000 population. GOI recognized leprosy as a national health problem, and launched the National Leprosy Control Program in 1954-55. The program gained momentum during the Fourth Five Year Plan period (1969-1974) after it was made a centrally sponsored program, thus receiving the necessary priority and funding. The program was expanded to cover additional populations in rural and urban areas at this time. To achieve this increased coverage, the involvement of NGOs was strengthened, and health education programs became a prominent component of the leprosy program. The government also encouraged the involvement of NGOs in SET (Survey Education and Treatment) activities in allotted areas through a scheme introduced in 1983. SET centers were set up in moderate/low endemic areas and urban leprosy centers in urban areas. These centers were staffed with one paramedical worker for a population of 25,000 called a sector, and there was one non-medical supervisor for every five paramedical workers. The paramedical worker conducted a house-to-house search for leprosy patients, “surveying” the entire population in a cycle of two years. Diagnosis followed cumbersome slit smear techniques, with treatment of confirmed cases lasting between 10 years and lifelong treatment.
The leprosy program provided free domiciliary treatment in endemic districts through specially trained staff in fixed leprosy control units; and in moderate to low endemic districts, through mobile leprosy treatment units. Cases were treated at monthly leprosy clinics held at a fixed point in the village. This led to improved compliance and provided an opportunity for counselling each patient. Patients were encouraged to come to the clinics with their families, and this helped address the issue of stigma. Educating communities to recognize the early signs and symptoms of leprosy was an integral part of the house-to-house visits made as part of SET activities. This was probably the origin of IEC in the program. India’s national leprosy control efforts began in 1955 with the National Leprosy Control Programme (NLCP) which was a vertical programme and relied on dapsone monotherapy as The monotherapy with Dapsone was started as domiciliary treatment for leprosy cases.
In 1982, the definitive cure for leprosy with Multi Drug Therapy (MDT) containing this bactericidal drug Rifampicin and bacteriostatic drug clofazimine besides dapsone was endorsed by WHO as the standard leprosy treatment regimen. In 1983 the introduction of MDT regimens marked the beginning of the National Leprosy Eradication Programme (NLEP).
Reflecting Mahatma Gandhi’s commitment to those affected by leprosy, India’s public health efforts have focused not just on treatment but also on mainstreaming affected individuals into society. Early detection and free treatment are core strategies, as delayed care can cause permanent disability.
Efforts Toward Elimination
The NLEP is a centrally sponsored scheme under the National Health Mission (NHM). Funds are allocated to states and UTs based on state/UT specific Programme Implementation Plans, with a focus on local needs, priorities, and capacity. Introduction of MDT, strong political commitment, decentralized implementation, and a robust Information, Education, and Communication (IEC) strategy brought about tremendous success in leprosy control. In 1981 the leprosy prevalence rate that was 57.2 /10,000 was reduced to 44.8 by March 1984 and to 2.4 per 10,000 population by March 2004. The rate of Grade II deformity (visible deformities) among new patients in 1981 was 20 percent; and by 2004, it was only 1.5 percent.
The World Bank’s support through two projects (1993–2000 and 2001–2004) emphasized community participation and funded IEC innovations. Partnerships with NGOs, WHO, Danida, and media agencies like BBC WST and SOMAC: Lintas enhanced outreach and message quality. Special focus was placed on women, tribal populations, and urban poor, addressing barriers to access and stigma. Integration with the general health system expanded reach, with Auxiliary Nurse Midwives (ANMs) and Anganwadi Workers (AWWs) playing key roles.
In March 2004, 17 states and 250 districts had achieved the goal of leprosy elimination (defined as a prevalence rate of less than one per 10,000 population) and 7 states were close to the goal. With determined campaigns to search for early leprosy cases, there has been a drastic reduction in the number of cases exhibiting these forms of the disease. The goal of bringing the deformity rate down to less than 2 percent by the end of the current World Bank supported project (2001-04) had been achieved. India as a whole achieved the goal of national elimination of leprosy by December 2005. India’s leprosy response under NLEP includes:
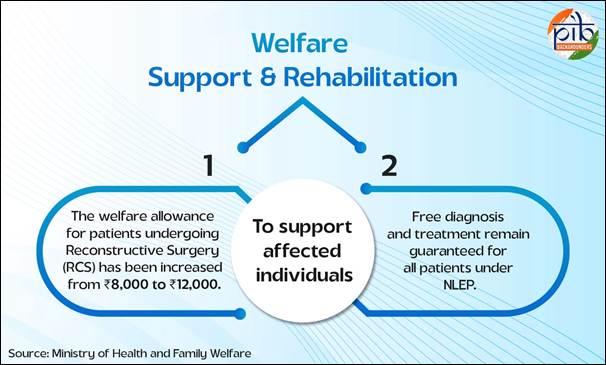
- Free diagnosis, treatment with MDT all patients and post exposure prophylaxis (PEP) with single dose rifampicin (SDR) provided to healthy contacts of patients under NLEP. Triple drug for both Pauci (PB) and Multibacillary (MB) patients introduced in 2025.
- Early Case Detection Campaigns-(i) Leprosy Case Detection Campaign (LCDC): Door-to-door surveys, especially in high-endemic areas (ii) Focused Leprosy Campaign: Targeted survey in villages and urban areas where a case of grade II disability or child case detected (iii) Special Plan for Hard-to-Reach areas and High-risk population (iv) Healthy Contact Examination of newly detected cases (v) Retrospective Contact Tracing and Examination for new cases detected in at least last five years (vi) ABSULE for low endemic area.
- Disability Prevention, Medical Rehabilitation (DPMR) and Welfare Support: Services include patient education and counselling for providing Micro Cellular Rubber (MCR) footwear, Self Care Kits, aids and appliances such as splints, crutches etc., effective management of ulcers and leprosy reactions, and reconstructive surgeries with compensation for loss of wages of ₹12,000.
- Capacity Building: Training of service providers -medical officers, laboratory technicians, physiotherapists, health supervisors, health workers and Accredited Social Health Activists (ASHAs).
- Community Awareness to promote voluntary reporting and stop stigma and discrimination: Sparsh leprosy awareness campaign around Anti-Leprosy Day and IEC as part of LCDC campaign are carried out annually to reduce stigma and promote early diagnosis.
- Abolishing Discriminatory Laws: NLEP is encouraging States and UTs towards abolishing all existing discriminatory laws against leprosy.
- Enhanced Surveillance and Notification of leprosy:
(i) Leprosy notification by all health sectors introduced in 2025 – Government, Private, NGOs, medical colleges etc.
(ii) ASHA-Based Surveillance for Leprosy Suspects (ABSULS) has strengthened case finding at the grassroots level.
- Digitalization of reporting systems-Digital reporting system Nikusth 2.0 introduced in 2023 for patient records and drug stock management.
Since 2015, constant efforts under NLEP have contributed to significant prevention of disability through early intervention and expanded surveillance mechanisms.
National Strategic Plan (NSP) and Roadmap for Leprosy 2023-2027
NLEP embarked upon developing a new strategy document to accelerate the efforts towards leprosy control and overcome the impact of the Covid pandemic. This Strategy is aligned with the Global Leprosy Strategy 2021-2030 and the WHO Roadmap for Neglected Tropical Diseases 2021-2030, aiming to achieve interruption of transmission of leprosy by 2030. The Strategy focuses on interruption of transmission and achieving zero indigenous cases by accelerating case detection activities in high endemic districts and sustaining a strong surveillance system in low endemic districts.
Strategies to be adopted are: (i) acceleration of new case detection by targeted approach; (ii) Intensified surveillance systems; (iii) digitalization; (iv) introduction of advanced tools and techniques for early diagnosis; (v) provide the immediate chemoprophylaxis to all contacts of cases forthwith; (vi) introduce a potential safe and effective vaccine; (vii) introduction of surveillance of anti-microbial resistance and adverse drug reactions; (viii)post treatment surveillance of treated cases and provide them care after cure; (ix)sustain leprosy expertise and move towards multi-disease service integration; (x) improved treatment outcomes by introduction of new treatment regimes; and (xi) widespread awareness with impactful behavioural change communication methods.
In addition, strengthening existing partnerships, adding more partners and repealing the existing discriminatory laws against leprosy is also required. The implementation of the National Strategic Plan and Roadmap for Leprosy 2023- 2027 for leprosy aims to achieve interruption of transmission at district level evidenced by zero occurrence of new child cases for at least five consecutive years. After achieving interruption of transmission, districts shall move on to achieve elimination of leprosy as a disease with zero new cases reported for at least three consecutive years. A follow up of those districts will be done side by side for verification.
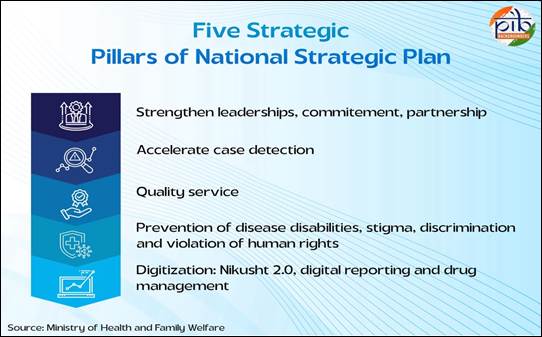
A “whole-of-government” and “whole-of-society” approach, along with digital surveillance tools, and strong institutional memory, are being employed for meeting the target.
Major Initiatives under NLEP
- National Strategic Plan and Roadmap for Leprosy 2023-27: The strategy document and roadmap outline the strategic interventions and lay out a clear-cut roadmap to achieve the goal of interruption in transmission of leprosy by 2027.
- Contact tracing is done and Post Exposure Prophylaxis (PEP) is administered to the eligible contacts of index case in order to interrupt the chain of transmission.
- Leprosy screening has been integrated with the activities of comprehensive primary health care under Ayushman Bharat Yojana for screening of people above 30 years of age.
- Leprosy screening has been integrated with Rashtriya Bal Swasthya Karyakram (RBSK) and Rashtriya Kishore Swasthya Karyakram (RKSK) for screening of children (0-18 years).
- Various services are being provided under the programme for Disability Prevention and Medical Rehabilitation (DPMR) i.e., reaction management, provision of Microcellular Rubber (MCR) footwear, Aids & Appliances, self-care kits etc.
- Nikusth 2.0: A revamped web-based ICT portal for data recording, reporting, and monitoring of leprosy activities for further strengthening services related to diagnosis, treatment, and follow-up of leprosy patients was launched on 30th January 2023 (National Anti-Leprosy Day) by Hon’ble Union Health Minister.
- National Anti-Microbial Resistance Surveillance for Leprosy Guidelines were launched during National Anti-Leprosy Day 2023 for strengthening the surveillance of resistant leprosy cases.
- National Framework for Integration of Mental Health Services for Leprosy patients and their families.
- Revised classification of Leprosy & treatment regimen for PB & MB Cases in India as adopted by MoHFW, GOI is introduced by Central Leprosy Division on 17th January 2024 & shall be implemented in all States/UTs from 1st April 2025. This treatment Regimen for leprosy patients will mark significant step forward in our collective efforts to eradicate leprosy in India by 2027.
- Implementation of tagging system for PVTGs within Nikusth 2.0 Portal for total of 17 states, as listed in Tribal Cell, which have been identified as having Particularly Vulnerable Tribal Groups (PVTGs) within their states under PM-JANMAN.
- Issued directions from Ministry to all states and UTs on Notification of Leprosy.
- Special monitoring framework for 121 Districts having Prevalence rate more than 1 per 10,000 population
- Focused strategies for Districts having PR >1 , High child and Disabilities.
Key Achievements and Program Outcomes under NLEP
- India achieved elimination status in March 2005 at the national level which means Prevalence Rate<1/10,000 population and sustained this till date. Since then, the programme is working towards achieving this goal at the sub national level.
- As of March 2025, 31 States and 638 districts have achieved Prevalence Rate <1 per 10,000 population.
- Over the years, India’s leprosy prevalence rate has reduced from 57.2 per 10,000 in 1981 and 0.69 per 10,000 in 2014–15 to 0.57 in 2024–25.
- The new case detection rate has also dropped from 9.73 per 100,000 in 2014–15 to 7.0 per 100,000 in 2024–25.
- Percentage of Child cases among new cases detected has gradually reduced from 9.04% in 2014-15 to 4.68% in 2024-25 indicating the programme efforts in reducing active transmission of leprosy in the community.
- Grade 2 disability per million population has also shown a decline from 4.68 case per million population in 2014-15 to 1.88 cases in 2024-25 reflecting case finding efforts among potential hidden cases.
- Preventive measure of Post Exposure Prophylaxis with single dose rifampicin (PEP-SDR) is administered to healthy contacts of leprosy cases. The percentage of eligible contacts administered has also increased from 71% in 2019-20 to 92% in 2024-25 in order to interrupt the chain of transmission.
- Intensified case search activities like LCDC have been conducted two times a year in high endemic states to facilitate identification of cases at an early stage. In F.Y. 2024-25, a total of 27,428 new cases were confirmed through LCDC.
- Enhanced integration with Rashtriya Bal Swasthya Karyakram (RBSK), Rashtriya Kishor Swasthya Karyakram (RKSK), and Ayushman Bharat ensures screening across all age groups.
State-wise NLEP Prevalence Rates per 10000 population as on March 2025
|
State/UT
|
PR/10,000
|
State/UT
|
PR/10,000
|
|
Andhra Pradesh
|
0.46
|
Nagaland
|
0.11
|
|
Arunachal Pradesh
|
0.15
|
Odisha
|
1.37
|
|
Assam
|
0.26
|
Punjab
|
0.14
|
|
Bihar
|
0.85
|
Rajasthan
|
0.14
|
|
Chhattisgarh
|
1.80
|
Sikkim
|
0.17
|
|
Goa
|
0.45
|
Tamil Nadu
|
0.26
|
|
Gujarat
|
0.38
|
Telangana
|
0.46
|
|
Haryana
|
0.13
|
Tripura
|
0.02
|
|
Himachal Pradesh
|
0.14
|
Uttar Pradesh
|
0.37
|
|
Jharkhand
|
1.46
|
Uttarakhand
|
0.22
|
|
Jammu & Kashmir
|
0.07
|
West Bengal
|
0.46
|
|
Karnataka
|
0.27
|
A & N Islands
|
0.19
|
|
Kerala
|
0.11
|
Chandigarh
|
1.35
|
|
Madhya Pradesh
|
0.82
|
DD & DNH
|
0.63
|
|
Maharashtra
|
1.12
|
Delhi
|
0.71
|
|
Manipur
|
0.05
|
Lakshadweep
|
0.14
|
|
Meghalaya
|
0.03
|
Ladakh
|
0.33
|
|
Mizoram
|
0.10
|
Puducherry
|
0.11
|
International Recognition & Partnerships
India has collaborated with WHO for supply of free MDT drugs, technical support, independent programme evaluation, capacity building and programme monitoring and supervision. In the World Health Assembly Commitment (1991), India committed to the World Health Assembly’s goal of eliminating leprosy as a public health problem by the year 2000. Although the national goal was extended to 2005, India made significant progress, with 17 states and 250 districts achieving elimination by 2004.
WHO supported India’s Modified Leprosy Elimination Campaigns (MLECs), diagnostic protocol shifts, and Special Action Projects for hard-to-reach populations. It also piloted the COMBI (Communication for Behavioural Impact) strategy in Bihar.
India has actively participated in developing Global Leprosy Strategies and global technical guidance documents. India has been part of the The Global Appeal since 2006 sharing an annual message to raise awareness and call for an end to the unjust discrimination that persons affected by leprosy continue to face. In the WHO India Country Co-operation Strategy under the umbrella of NTD control and elimination, leprosy remains a priority area for WHO’s technical support in India. This includes strengthening surveillance and case detection, supporting post-exposure prophylaxis (PEP), reducing stigma and discrimination and enhancing access to treatment and rehabilitation. In the Weekly Epidemiological Report of Global leprosy situation, 2006, India was dropped from the list of countries that had not achieved elimination of leprosy as a public health problem.
In 2023, the World Health Organization (WHO) acknowledged India’s 2005 milestone of eliminating leprosy as a public health problem, underscoring the country’s progress in disease control. Additionally, India continues to collaborate actively with global partners, including the WHO, the International Federation of Anti-Leprosy Associations (ILEP), and various non-governmental organizations (NGOs), which offer both technical expertise and financial assistance to strengthen India’s leprosy elimination initiatives. ILEP and other partner NGOs: NLEP has also collaborated with ILEP organizations, Sasakawa Health Foundation, The World Bank, Global Partnership for Zero Leprosy (GPZL), Hind Kushth Nivaran Sangh and other NGO partners such as ALERT India, IAL, IADVL, BLP, Schieffelin Institute Karigiri, International Leprosy Union etc. in improving community awareness and quality diagnostic, therapeutic and rehabilitative services. India’s efforts in combating leprosy have received significant international recognition and support.
India’s journey with leprosy control is a remarkable story of successful disease control. From a prevalence rate of 57.2 per 10,000 population and 39.19 lakh patients on treatment, India in 2025 has a prevalence rate of 0.57 and 0.82 lakh patients on treatment. This depicts a drop in prevalence rate of 99% and 98% drop in cases under treatment over a span of 44 years. There has been a decline of 37% in new case detection since March 2006 when the annual report confirmed a prevalence rate of less than 1 per 10,000 (0.84).
NLEP Programme demonstrates a public health success rooted in political will, commitment, sustained efforts for new case detection, free of cost and uninterrupted supply of MDT drugs, partner support, transition from a vertical to integrated service delivery strategy, timely adoption of global guidance, timely introduction of revised treatment regimens, post exposure prophylaxis, innovations, and expanding community engagement. However, elimination as a public health problem is not eradication. New cases of leprosy will continue to occur and the aim is to detect cases so early that development of disabilities is prevented and chain of transmission is interrupted leading to no new infections and no leprosy in children.
Recognizing this, the Government has been proactively addressing residual challenges through sustained surveillance, renewed awareness initiatives, and enhanced community outreach. Efforts are underway to revitalize training programs and improve early detection, especially in rural, tribal and underserved populations, ensuring that no case goes unreported or untreated.
With ongoing efforts to strengthen surveillance systems, expand community engagement, and integrate leprosy care into general health services, India is reinforcing its commitment to a leprosy-free future. Technological tools like Nikusth 2.0, combined with strong policy support, post exposure prophylaxis and increased community participation and self-reporting. NSP and Roadmap for Leprosy provides a comprehensive framework aligned with global goals to achieve interruption of transmission by 2030 through accelerated case detection, digital surveillance, improved treatment, preventive strategies, and strong partnerships, aiming ultimately for elimination of leprosy in India. As India approaches its goal of zero transmission, continued political will, adequate funding, and active public involvement will be key. With these in place, the country is well-positioned to achieve not just a medical milestone but a lasting humanitarian achievement.
Ministry of Health and Family Welfare
https://dghs.mohfw.gov.in/nlep.php
https://dghs.mohfw.gov.in/nlep.php
https://nhm.gov.in/index4.php?lang=1&level=0&linkid=281&lid=348
https://nlrindia.org/wp-content/uploads/2024/03/NSP-Roadmap-for-Leprosy-2023-2027.pdf
Press Information Bureau
https://www.pib.gov.in/PressReleasePage.aspx?PRID=1738154
World Health Oganization
https://www.who.int/activities/monitoring-the-global-leprosy-situation
Other Links
https://documents1.worldbank.org/curated/en/428771468033300814/pdf/320410MukherjiLeprosyFinal.pdf
https://www.who.int/publications/i/item/who-wer8132
Click here to see PDF
SK/M
(रिलीज़ आईडी: 2174943)
आगंतुक पटल : 5102