PIB Headquarters
Understanding Mental Health
Global Perspectives and Indian Initiatives
Posted On:
09 NOV 2025 3:05PM by PIB Delhi
Mental well-being is more than about being happy or in a good mood — it encompasses all our mental-emotional, social, cognitive and physical capabilities. Navigating through life’s challenges and living life to the fullest is more probable if we take care of our mental health.
Mental health is a basic human right and is crucial for personal, community and socio-economic development.2 Over the past few years, there has been enhanced focus on and increased discussion of mental health issues. While there has been a sharp attention on mental health for more than a decade among the various medical, counselling, patient and other communities connected with this sector, the global COVID-19 pandemic with its widespread impact appears to have served as a catalyst for refocusing attention on this issue (United Nations, 2021).

According to WHO, mental health conditions are among the leading causes of disability worldwide. In 2021, it was estimated that 1 in 7 people globally were living with a mental disorder, which equates to over 1.1 billion people. In India, about 11 in 100 people suffer from mental health disorders.
 The impact of these conditions is particularly evident in terms of years lived with disability (YLD), with depression and anxiety disorders being major contributors across all age groups except 0-5 year olds and especially among 15-29 year olds (WHO,2025).
The impact of these conditions is particularly evident in terms of years lived with disability (YLD), with depression and anxiety disorders being major contributors across all age groups except 0-5 year olds and especially among 15-29 year olds (WHO,2025).
According to a Lancet study (2020), mental health disorders account for 5.2% of the global disease burden, with depressive disorder and anxiety disorder alone contributing to 6.2% and 4.7% respectively, of the total YLD (Mental Health Atlas, 2024). This growing burden underscores the escalating challenge mental health issues pose to health systems globally.
The Government of India has taken initiative in filling the treatment gaps, disease burdens, and the extent of disabilities due to mental illness (National Health Policy, page 4). It is addressing the illness through its various policies and programmes.
Types of Mental Health Illnesses

Mental Health in India
About 10.6% of Indian adults – roughly 11 out of every 100 adults – were living with a diagnosable mental health disorder, according to a 2015-16 National Mental Health Survey (NMHS) conducted by the National Institute of Mental Health and Neurosciences (NIMHANS).
The survey also revealed:
- 15% of India’s adult population experiences mental health issues requiring intervention
- The lifetime prevalence of mental disorders was 13.7%, indicating that around 14 out of every 100 people in India have experienced a mental disorder at some point in their lives
- Mental health disorders are more prevalent in urban areas (13.5%), compared to rural areas (6.9%).
According to a NIMHANS study from 2019, mental health disorders are more prevalent among women (20%) than men (10%). Women in India are found to be particularly more prone to conditions like depression, anxiety, and somatic complaints compared to their male counterparts.
Suicide rates in India are on the rise. According to the 2023 National Crime Records Bureau (NCRB) report ‘Accidental Deaths & Suicides in India’:
- 171,418 suicides were reported in the country in 2023.
- The 2023 NCRB report revealed a significant gender disparity in suicides: males accounted for 72.8% of all suicides, while females accounted for 27.2%.
Treatment Gap
The 2015-16 NIMHANS survey also highlighted that 70% to 92% of people with mental disorders do not receive proper treatment due to the lack of awareness, social stigma, and a shortage of professionals.
Lack of mental healthcare professionals also plays a role. While the WHO recommends at least 3 psychiatrists per 100,000 people, according to a study by Garg et al., published in the Indian Journal of Psychiatry in 2019, India has 0.75 psychiatrists per 100,000 people.
Impact of Poor Mental Health
Poor mental health has wide-ranging impacts on people’s health and socio-economic development.
Physical Health
The World Health Organisation emphasises that there is a strong correlation between mental and physical health – individuals with poor mental health face poorer overall health and have shorter life expectancy. For example, people with depression are at a higher risk of developing conditions like cardiovascular diseases, with one Lancet Psychiatry study saying that the risk rises by 72% (Viola V et al., 2025). Chronic pain and sleep disturbances are also prevalent in people with poor mental health.
Economic Impact
Poor mental health of workers indirectly decreases economic output – it leads to productivity losses (absenteeism, presenteeism, and staff turn-over) and other indirect costs to society far outstrip healthcare costs (WHO, 2025). These, in turn, lead to a reduction in people’s earning potential and growth, increase unemployment rates, and lead to greater healthcare costs. (Sartorius, 2013). It is estimated that depression and anxiety cost the global economy nearly US$1 trillion annually in lost productivity (WHO, 2025).
The global financial burden of mental health conditions, which includes healthcare and indirect costs, is expected to rise to $16 trillion by 2030 (Journal of Mental Health, 2021). The generational effects are notable too, as children of individuals with mental health conditions are at increased risk of facing economic disadvantages, including poorer educational outcomes and lower lifetime earnings (Doran & Kinchin, 2019).
Social and Relationship Strains
People with mental health problems are at risk of becoming socially isolated, with strained relationships and communication challenges adding to the obstacles they face. A study published in The Lancet Psychiatry (2010) revealed that individuals with depression face difficulties in forming and maintaining interpersonal relationships, which can intensify depression symptoms due to a lack of social support.
Social Stigma
Stigma – which includes internalised shame and negative beliefs as well as structural stigma related to lack of mental health care and policies – associated with mental health is a major obstacle to seeking treatment and social integration (American Psychiatric Association, 2024).
People in low- and middle-income countries, especially, are more vulnerable to the vicious cycles of isolation and worsening mental health because of the stigma associated with seeking mental health care (WHO, 2018). For example, a study published in The Lancet Psychiatry (2020) found that individuals with mental health disorders, particularly those with severe conditions like schizophrenia, are frequently subject to discrimination and marginalisation. The lack of care diminishes the quality of their lives and decreases any chance of treatment or recovery.
Increased Suicide Risks
Globally, over 727,000 people die by suicide each year (WHO, 2025). According to a study published in Psychiatry Research (2023), individuals with mental disorders face a 16-fold higher risk of suicide compared to those without such conditions, with this elevated risk remaining consistent across regions and time periods.
Younger People Are More Vulnerable
About one third of the mental disorders that adults experience actually began by age 14, and half started by age 18, and nearly two thirds had their onset by age 25 (WHO,2025) Mental health disorders frequently manifest during childhood or adolescence, with 50% of all mental health conditions appearing by age 14 and 75% by age 24 (WHO, 2020). A study published in The Lancet (2017) shows that mental health issues in adolescence are associated with poor academic outcomes, increased substance use, and higher rates of self-harm, highlighting the long-term impact of untreated mental health problems in young people.
Impact of COVID-19 on Mental Health
The COVID-19 pandemic has had profound effects on global mental health. Key impacts include:
- Increased Anxiety and Depression: The number of individuals affected by anxiety disorders rose by about 25% during the pandemic.
- Social Isolation: Quarantine measures led to significant feelings of loneliness and despair among various populations.
- Economic Stress: Job losses and financial insecurity contributed to heightened stress levels and deteriorating mental health conditions.
Global Policy Frameworks
All WHO Member States are committed to implementing the “Comprehensive Mental Health Action Plan 2013-2030”, which aims to improve mental health by strengthening effective leadership and governance, providing comprehensive, integrated and responsive community-based care, implementing promotion and prevention strategies, and strengthening information systems, evidence and research.
In 2022, the WHO released the "World Mental Health Report," which calls for transformative actions to improve mental health globally. The Report outlines several transformative strategies aimed at improving mental health care globally.
Here are the key suggestions:
Three Paths to Transformation:
- Deepen Value and Commitment: Encourage individuals and societies to recognize the intrinsic value of mental health, promoting social inclusion and prioritising mental health alongside physical health.
- Reshape Environments: Modify physical, social, and economic environments to promote better mental health outcomes. This includes enhancing conditions in homes, schools, workplaces, and communities.
- Strengthen Mental Health Care: Transition from custodial care in psychiatric hospitals to community-based care models. This involves building networks of interconnected services that integrate mental health care into general healthcare systems. Diversify and scale up care options for common mental health conditions like anxiety and depression, utilizing task-sharing approaches and digital technologies to enhance accessibility and effectiveness of care (WHO, 2022).
The WHO Report also recommends several strategies for integrating mental health care into Universal Health Coverage (UHC).

WHO emphasises that integrating mental health care into UHC can significantly improve overall health outcomes, reduce treatment gaps, and enhance the quality of life for individuals with mental disorders globally.
Various promotion and prevention programs, particularly in the health sector can contribute significantly by embossing promotion and prevention efforts within health services and by advocating, initiating and facilitating multisectoral collaboration and coordination.8
India’s Comprehensive Push for Mental Health
Policies
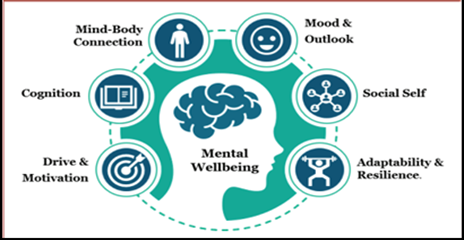
National Mental Health Programme (NMHP) – 1982
Launched in 1982 to address the growing burden of mental disorders and shortage of mental health services in India.
Primary Goal: Integrate mental healthcare into general healthcare system and make it accessible to all, especially vulnerable and underprivileged groups.
District Mental Health Programme (DMHP) – 1996
Integrated into NMHP in 1996, based on Karnataka's 'Bellary Model'.
Coverage: Started in 4 districts (1996), expanded to 27 districts during IX Five Year Plan, now covers 767 districts.
Services Provided:
- Counseling and outpatient treatment
- 10-bedded inpatient facilities at district level
- Suicide prevention initiatives
- Awareness programs
Team Composition per District: Psychiatrist, clinical psychologist, psychiatric social worker, psychiatric/community nurse, monitoring & evaluation officer, case registry assistant, ward assistant/orderly.
Key Components:
- Early detection and treatment
- Short-term training for general physicians
- Training for health workers to identify mental illness
- Public awareness (IEC) campaigns
- Simple record-keeping for monitoring
Approach: Community-based model focusing on training health workers, reducing stigma, providing early intervention, and collecting data for service planning and research.
National Suicide Prevention Strategy (NSPS) – 2022
Launched by the Ministry of Health and Family Welfare in 2022.
Goal: Reduce suicide mortality by 10% by 2030.
Key Components:
- Mental health screenings in schools and colleges
- Establishing Crisis helplines and psychological support centers
- Community awareness programs to break stigma
- Workplace mental health programs
Target Groups: Students, farmers, young adults, and other high-risk populations for targeted intervention and prevention.
Training, Infrastructure, and Digital Innovation
Training of Mental Healthcare Professionals
Infrastructure Development:
- 47 government-run mental hospitals (3 central institutions: NIMHANS Bengaluru, LGBRIMH Tezpur, CIP Ranchi; 44 state-run hospitals)
- Mental health services available across all AIIMS facilities
Manpower Development Scheme A - Centers of Excellence:
- Total: 25 CoEs sanctioned to strengthen courses in psychiatry, clinical psychology, psychiatric social work, and psychiatric nursing
- 11th Plan (2007-2012): 11 CoEs @ Rs. 30 crore each
- 12th Plan (2012-2017): 10 CoEs @ Rs. 33.70 crores each
- Beyond 12th Plan (2017-2018): 4 CoEs @ Rs. 36.96 crores each
- Grant covers capital work, equipment, furnishing, and faculty retention
- Provides tertiary-level care, creates PG seats, conducts research, and supports DMHP implementation
Manpower Development Scheme B - PG Department Upgradation:
- Total: 47 PG Departments in 19 government institutions
- 11th Plan (2009-2011): 27 Departments in 11 institutes @ Rs. 51 lakhs to 1 crore
- 12th Plan (2015-2016): 13 Departments in 4 institutes @ Rs. 0.85-0.99 crores each
- Beyond 12th Plan (2017-2018): 7 Departments in 4 institutes @ Rs. 1.89-2.20 crores each
Digital Training Initiatives:
- Digital Academies (since 2018): Established at NIMHANS, LGBRIMH, and CIP Ranchi; trained 1,76,454 healthcare professionals
- iGOT-Diksha Platform (2020): Trained healthcare professionals, frontline workers, and community volunteers; enhanced grassroots capacity
Strengthening Mental Health Care through Ayushman Bharat
Recognising mental healthcare as a vital component of overall well-being, India has taken a major step toward universal health coverage by integrating mental health services into primary care through Ayushman Arogya Mandirs under the Ayushman Bharat initiative.
Under the Ayushman Bharat initiative, over 1.75 lakh Sub Health Centres (SHCs) and Primary Health Centres (PHCs) have been upgraded into Ayushman Arogya Mandirs, where mental health services are now an integral part of Comprehensive Primary Health Care. This integration ensures accessible and inclusive mental health support at the grassroots level. Key highlights include:
- Integrated Mental Health Services: Mental healthcare has been integrated as a core component of the primary care services provided at Ayushman Arogya Mandirs.
- Financial Protection: Through Ayushman Bharat PM-JAY, mental health conditions are covered under a Rs. 5 lakh per family annual insurance, with over 1.35 lakh admissions worth Rs. 120.19 crore authorized between FY 2021-22 to FY 2023-24 (Parliament of India, Unstarred question, 2023).
- Under the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana initiative, provides cashless healthcare services, including 22 procedures under Mental Disorder speciality such as Intellectual Disability, Schizophrenia, schizotypal, delusional disorders, autism spectrum disorder, etc. Further, States have been provided flexibility to further customize the Health Benefit Packages to the local context. (Press Information Bureau, March 25th, 2024).
- Additionally, the initiative provides coverage for various treatments and interventions related to these disorders, including counselling and psychiatric care. The inclusion of these conditions aims to reduce the treatment gap and ensure that individuals receive necessary mental health services without facing financial burdens.
- Telepsychiatry Access: Telemedicine, especially via Tele MANAS, enhances access to mental health services in underserved regions.
- Capacity Building & Awareness: Health workers are being trained to diagnose and manage mental illnesses, supported by public campaigns to reduce stigma and promote mental well-being.
- Expanded District Mental Health Program (DMHP) Services: Community and Primary Health Centres offer outpatient care, counselling, medications, outreach, and emergency support under the District Mental Health Program.
COVID-19 Response (2020)
During the pandemic, the Ministry of Health and Family Welfare launched a 24/7 national helpline (080-4611 0007) to provide psychosocial support and counselling for individuals affected by stress, anxiety, and other mental health challenges (Press Information Bureau, 2021).
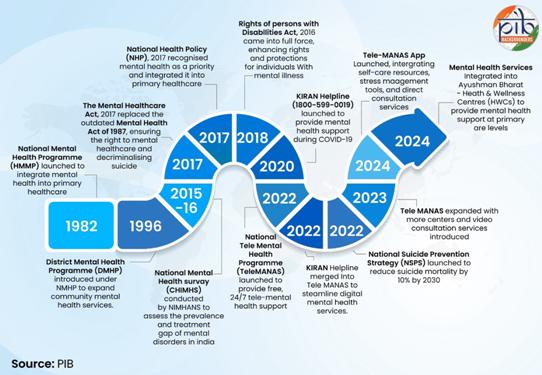
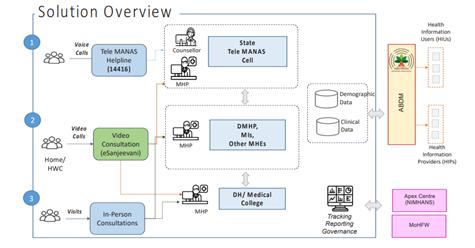
Tele MANAS Mobile App & Video Consultation
Tele MANAS - Toll-Free Mental Health Service
Launched: World Mental Health Day, 2022
Coverage: All 36 states and union territories
Toll-Free Numbers:
Usage: 2,838,322 calls handled (as on October 27, 2025)
Tele MANAS Mobile App
Features:
- Information library with self-care tips
- Guidance on recognizing distress signals
- Managing stress, anxiety, and emotional struggles
- Confidential support through trained counsellors and mental health professionals across India
Video Consultation (VC) Feature
Launch: October 10, 2024 (Pilot)
Pilot States: Karnataka, Tamil Nadu, Jammu & Kashmir
Nationwide launch: 16th June, 2025
Functionality:
- Mental Health Professionals (psychiatrist, clinical psychologist, psychiatric social worker, psychiatric nurse) can escalate audio consultations to video based on clinical need
- Only psychiatrists are authorized to issue e-prescriptions
Usage: 1242 video calls handled (as of October 27, 2025)
Recognition
WHO Endorsement: World Health Organisation has recognized Tele MANAS as an innovative and effective model for delivering mental health care.
WHO Representative to India, Dr. Roderico H. Ofrin (at October 2024 app launch) highlighted the initiative's potential to enhance mental health outcomes and emphasized the role of Ayushman Arogya Mandirs as a key pillar of India's public health system.


Source: “Rapid assessment report on Tele MANAS: Tele Mental Health Assistance and Networking Across States”, Ministry of Health and Family Welfare, 2024.
Recent developments
Recognizing the critical role of mental health, the Economic Survey 2024–25 underscored that mental well-being encompasses mental-emotional, social, cognitive, and physical dimensions. It advocated for a ‘whole-of-community’ approach to addressing mental health challenges and stressed the urgent need for viable, impactful preventive strategies and interventions. The survey emphasised that India’s demographic dividend depends not only on skills, education, and physical health, but most importantly, on the mental well-being of its youth. Key recommendations from the survey included:
- Strengthening Mental Health Education in Schools: Implement early intervention strategies to address anxiety, stress, and behavioural issues among students.
- Enhancing Workplace Mental Health Policies: Tackle job-related stress, long working hours, and burnout through supportive policies.
- Scaling Up Digital Mental Health Services: Strengthen Tele MANAS and incorporate AI-powered mental health solutions.
Mental health remains a pressing global challenge with profound impact on individuals and economies, disproportionately affecting vulnerable populations. While India has made significant strides through initiatives like Tele MANAS and the National Mental Health Programme, building a mentally healthier society requires strengthening awareness, expanding workforce training, investing in digital solutions, and adopting a whole-of-society approach to ensure accessible, inclusive, and stigma-free mental healthcare for all.
Manisha Verma
Former ADG (Media)
Ministry of Health and Family Welfare
References
American Psychiatric Association. (2024). Stigma, prejudice and discrimination against people with mental illness. Retrieved May 20, 2025, from https://www.psychiatry.org/patients-families/stigma-and-discrimination
Doran, C. M., & Kinchin, I. (2019). A review of the economic impact of mental illness. Australian Health Review, 43(1), 43–48. Retrieved May 20, 2025, from https://doi.org/10.1071/AH16115
Galderisi, S., Heinz, A., Kastrup, M., Beezhold, J., & Sartorius, N. (2015). Toward a new definition of mental health. World Psychiatry, 14(2), 231–233. Retrieved March 22, 2025, from https://doi.org/10.1002/wps.20231
Garg, K., Kumar, C. N., & Chandra, P. S. (2019). Number of psychiatrists in India: Baby steps forward, but a long way to go. Indian Journal of Psychiatry, 61(1), 104–105. Retrieved May 23, 2025, from https://doi.org/10.4103/psychiatry.IndianJPsychiatry_7_18
Government of India, Ministry of Health and Family Welfare. (2014). National Mental Health Policy of India: New Pathways, New Hope. Ministry of Health and Family Welfare. Retrieved May 20, 2025, from https://nhm.gov.in/images/pdf/National_Health_Mental_Policy.pdf
Horton, R. (2021). Offline: The pandemic and the politics of health. The Lancet, 398 (10307), 1–2. Retrieved April 17, 2025, from https://doi.org/10.1016/S0140-6736(21)02143-7
India State-Level Disease Burden Initiative Mental Disorders Collaborators. (2020). The burden of mental disorders across the states of India: the Global Burden of Disease Study 1990–2017. The Lancet Psychiatry, 7(2), 148–161. Retrieved March 25, 2025, from https://doi.org/10.1016/S2215-0366(19)30475-4
International Association for Suicide Prevention. (2023, December 11). Universal Health Coverage Day 2023. Retrieved April 28, 2025, from https://www.iasp.info/2023/12/11/universal-health-coverage-day-2023/
International Labour Organization. (2022, September 28). WHO and ILO call for new measures to tackle mental health issues at work. https://www.ilo.org/resource/news/who-and-ilo-call-new-measures-tackle-mental-health-issues-work-0
Meghalaya Department of Health & Family Welfare. (2022). Meghalaya Mental Health and Social Care Policy, 2022. Retrieved April 28, 2025, from https://meghealth.gov.in/docs/Draft%20Meghalaya%20State%20Mental%20Health%20Policy%20(Oct%2010,%202022).pdf
Meghrajani, V. R., Marathe, M., Sharma, R., Potdukhe, A., Wanjari, M. B., & Taksande, A. B. (2023). A comprehensive analysis of mental health problems in India and the role of mental asylums. Cureus, 15(7), e42559. Retrieved May 24, 2025, from https://doi.org/10.7759/cureus.42559
Meghrajani, Vanee R., et al. "A Comprehensive Analysis of Mental Health Problems in India and the Role of Mental Asylums." Cureus, vol. 15, no. 7, 27 July 2023, e42559. PubMed Central, doi:10.7759/cureus.42559
Mental Health." World Health Organization, 8 Oct. 2025, www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response.
Ministry of Finance, Government of India. (2025). Economic Survey 2024-25. Retrieved May 27, 2025, from https://www.indiabudget.gov.in/economicsurvey/
Ministry of Health and Family Welfare. (2024). Rapid assessment report on Tele MANAS: Tele Mental Health Assistance and Networking Across States. Government of India. Retrieved May 27, 2025, from https://mohfw.gov.in/sites/default/files/Rapid%20Assessment%20report%20on%20TeleMANAS.pdf
National Crime Records Bureau. (2022). Accidental deaths & suicides in India – 2022. Ministry of Home Affairs, Government of India. Retrieved May 18, 2025, from https://ncrb.gov.in/uploads/files/AccidentalDeathsSuicidesinIndia2022v2.pdf
National Crime Records Bureau. (2023). Accidental deaths & suicides in India 2023. Ministry of Home Affairs, Government of India.
National Mental Health Programme. (n.d.). National Mental Health Programme. Ministry of Health and Family Welfare, Government of India. Retrieved May 25, 2025, from https://dghs.mohfw.gov.in/national-mental-health-programme.php
Parliament of India. (2023, December 15). Unstarred question no. 2196: Mental health coverage under Ayushman Bharat Pradhan Mantri Jan Arogya Yojana. Lok Sabha Secretariat. Retrieved May 27, 2025, from https://sansad.in/getFile/loksabhaquestions/annex/1714/AU2196.pdf
Press Information Bureau. (2021, March 9). COVID-19 helplines for mental health assistance. Ministry of Health and Family Welfare, Government of India. Retrieved May 27, 2025, from https://www.pib.gov.in/PressReleasePage.aspx?PRID=1703446
Press Information Bureau. (2024, October 13). Tele MANAS: Revolutionizing mental health care in India—Over 14.7 lakh calls served in two years, transforming mental healthcare accessibility. Ministry of Health and Family Welfare, Government of India. Retrieved May 27, 2025, from https://www.pib.gov.in/PressNoteDetails.aspx?NoteId=153277&ModuleId=3
Press Information Bureau. (2025, August 1). Steps taken to improve mental healthcare. Government of India. https://www.pib.gov.in/PressReleasePage.aspx?PRID=2151235
Press Information Bureau. (2025, February 7). Measures taken to improve mental healthcare. Ministry of Health and Family Welfare, Government of India. Retrieved May 27, 2025, from https://www.pib.gov.in/PressReleaseIframePage.aspx?PRID=2100593
Press Information Bureau. (2025, March 25). Steps taken on mental health. Ministry of Health and Family Welfare, Government of India. Retrieved May 27, 2025, from https://www.pib.gov.in/PressReleseDetailm.aspx?PRID=2114756
Rothenberger, S. D. (2020). The role of gender in mental health: How societal expectations impact psychological well-being. International Journal of Social Psychiatry, 66(5), 425-434. Retrieved April 28, 2025, from https://doi.org/10.1177/0020764020955594
Sagar, R., Dandona, R., Gururaj, G., Dhaliwal, R. S., Singh, A., Ferrari, A., ... & Dandona, L. (2020). The burden of mental disorders across the states of India: The Global Burden of Disease Study 1990–2017. The Lancet Psychiatry, 7(2), 148–161. https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(19)30475-4/fulltext?onwardjourney=584162_v1
Sanftenberg, L., Bentrop, M., Jung-Sievers, C., Dreischulte, T., & Gensichen, J. (2024). Videocall delivered psychological interventions for treating depressive symptoms in primary care – a systematic review. Expert Review of Neurotherapeutics, 24(12), 1261-1271. Retrieved May 24, 2025, from https://doi.org/10.1080/09638237.2024.2426985
Santomauro, D. F., Herrera, A. M. M., Shadid, J., Zheng, P., Ashbaugh, C., Pigott, D. M., ... & Whiteford, H. A. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet, 398(10312), 1700–1712. Retrieved May 23, 2025, from https://doi.org/10.1016/S0140-6736(21)02143-7
Shafie, S., Subramaniam, M., Abdin, E., Vaingankar, J. A., Sambasivam, R., Zhang, Y., Shahwan, S., Chang, S., Jeyagurunathan, A., & Chong, S. A. (2020). Help-Seeking Patterns Among the General Population in Singapore: Results from the Singapore Mental Health Study 2016. Administration and Policy in Mental Health and Mental Health Services Research, 48(4), 586–596. Retrieved May 23, 2025, from https://doi.org/10.1007/s10488-020-01092-5
Smith, J., & Doe, A. (2023). Exploring the effects of mindfulness on mental health. Journal of Psychosomatic Research, 161, 110442. Retrieved May 23, 2025, from https://doi.org/10.1016/j.jpsychores.2023.110442
Sutar, R., Kumar, A., & Yadav, V. (2023). Suicide and prevalence of mental disorders: A systematic review and meta-analysis of world data on case-control psychological autopsy studies. Psychiatry Research, 329, 115492. Retrieved May 24, 2025, from https://doi.org/10.1016/j.psychres.2023.115492
UNICEF India. (2024). Mental well-being for young people. https://www.unicef.org/india/mental-well-being-young-people
United Nations. (2021, October 9). The pandemic accelerant: How COVID-19 advanced our mental health priorities. United Nations. Retrieved March 23, 2025, from https://www.un.org/en/un-chronicle/pandemic-accelerant-how-covid-19-advanced-our-mental-health-priorities
Vaccarino, V., Prescott, E., Shah, A. J., Bremner, J. D., Raggi, P., Dobiliene, O., ... & Bugiardini, R. (2025). Mental health disorders and their impact on cardiovascular health disparities. The Lancet Regional Health–Europe, 56.
Vishwakarma, D., Gaidhane, A. M., & Choudhari, S. G. (2022). The Global Impact of COVID-19 on Mental Health of General Population: A Narrative review. Cureus. Retrieved April 17, 2025, from https://doi.org/10.7759/cureus.30627
World Health Organization. (2021). SDG target 3.4: Noncommunicable diseases and mental health. World Health Organization. Retrieved March 23, 2025, from https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/sdg-target-3.4-noncommunicable-diseases-and-mental-health
World Health Organization. (2022). World mental health report: Transforming mental health for all. World Health Organization. Retrieved March 28, 2025, from https://www.who.int/publications/i/item/9789240049338
World Health Organization. (2024, September 2). Mental health at work. https://www.who.int/news-room/fact-sheets/detail/mental-health-at-work
World Health Organization. (2025). Mental health atlas 2024. World Health Organization.
World Health Organization. (2025). World mental health today: latest data. World Health Organization.
World Health Organization. (n.d.). Suicide data. Retrieved April 28, 2025, from https://www.who.int/teams/mental-health-and-substance-use/data-research/suicide-data
*******
(Release ID: 2188003)
Visitor Counter : 8587